Cornea / External Eye Diseases
An easy way to understand the function of the cornea is to think about the eye as a camera. The cornea would be the glass on the front of the lens.
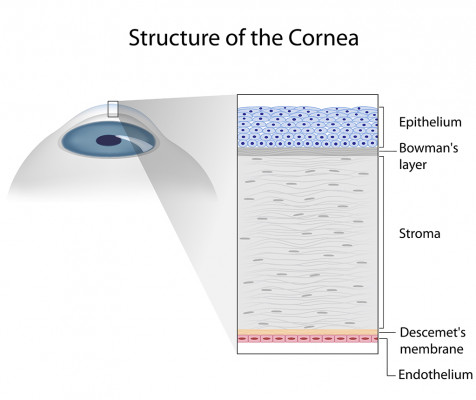
The cornea is a clear "window" through which light passes into the eye. It provides most of the focusing power. Corneal injury, disease, or hereditary conditions can cause clouding, distortion, and scarring.
Corneal clouding, similar to frost on a window-pane or dirty smudges on a camera lens, block the clear passage of light into the retina, reducing sight sometimes even to the point of blindness. Corneal injury and disease can sometimes be intensely painful.
What can cause corneal injury?
Nearly any foreign object can injure the eye, especially the cornea, the most exposed part of the eye. Protection of the cornea is the reason emergency washing of the eye is absolutely necessary when the eye is exposed to toxic chemicals. Most corneal injuries are preventable with protective glasses and proper precautions when dealing with hazardous substances.
What causes corneal disease and degeneration?
Infections, whether bacterial, fungal, or viral are frequent causes of severe corneal damage and ulceration. Abnormal steepening of the cornea (keratoconus), degeneration occasionally following cataract surgery (corneal edema or swelling), and some aging processes can also affect the clarity and health of the cornea.
Some disorders of the cornea are inherited and can lead to clouding and loss of sight.
Learn about Treatments for Corneal Disorders
To schedule an appointment, call (509) 456-0107
In the news
June 26, 2025
The Sun, UV Light and Your Eyes
Summer is here! It's hot outside, and the UV rays are high. Your skin isn't the only thing that needs protection, your eyes do, too! Here are some of the best practices for protecting your eyes this summer...
June 12, 2025
IMPORTANT! Fireworks Eye Safety
The numbers are clear: Fireworks are dangerous, and July 4 is especially risky for eye injuries.
According to the U.S. Consumer Product Safety Commission's most recent study on annual fireworks injuries, fireworks caused 8 deaths and 9,700 injuries in 2023. Nearly 66% of fireworks injuries treated in emergency rooms occurred from mid-June to mid-July...
